Neurosurgery
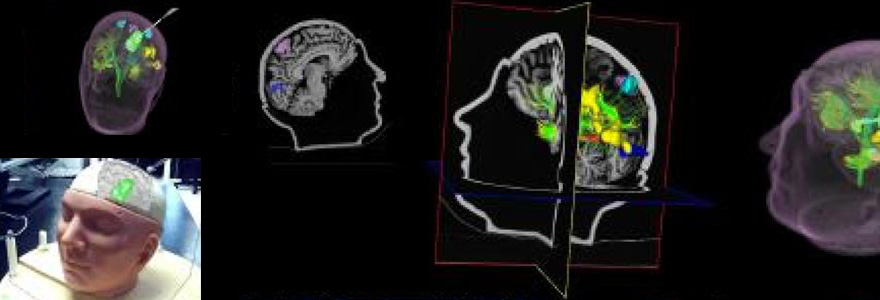
Image-Guided Neurosurgery
Current Graduate Students: Charlotte Blinston, John Baxter, Jonathan McLeod, Utsav Pardasani
Accurate frame-based stereotaxy depends on:
- Positioning - The position of the frame must be precise.
- Reducing Spatial Errors - Minimizing this type of error depends on the type of imaging modality used. We are currently investigating the use of MRI versus ultrasound.
- Frame Properties - The frame itself has
mechnanical properties thatinfluences accuracy. - Target computation - Algorithms used for target computation rely on the accurate selection of fiducial points in the image. Errors in the selection of these points will propagate through the computation to degrade the final result. This is the largest source of application error.
Our Contribution
In our laboratory, we present
This technique has a particular application to MR where the algorithm's automatic monitoring of image acquisition quality minimizes errors.
Using ultrasound guidance
Because the brain shifts position when craniotomy procedure is performed, image-guided surgery systems that rely on a pre-operative MR image are insufficient for a broad range of neurosurgical tasks. We are currently developing techniques that use ultrasound images of the brain, collected during the surgery, to track the distortion of the brain tissue. Once the distortion has been measured, we can use it to warp the pre-operative MR images. This helps to accurately reflect the shape of the brain during surgery.
How are 3D ultrasound image volumes constructed?
To create 3D ultrasound image volumes, the video from the tracked ultrasound probe is reconstructed using a real-time reconstruction technique. The ultrasound volume is built up step-by-step as the video frames are acquired. The ultrasound can be visualized through volume rendering techniques, or painted over the three MR image planes.
MRI vs. Ultrasound Video
We compare the ultrasound images to an MR image volume that was acquired prior to surgery. In order for this to be done, the ultrasound probe must be tracked in 3D space to monitor
The MR image is re-formatted in real time as the ultrasound operator moves the probe.
Because the overlay is done in real time (10 frames per second), the surgeon is able to very rapidly obtain a qualitative assessment of the shift. If the shift is not significant, then the surgeon has the option to immediately continue the surgery without any shift correction.