Research
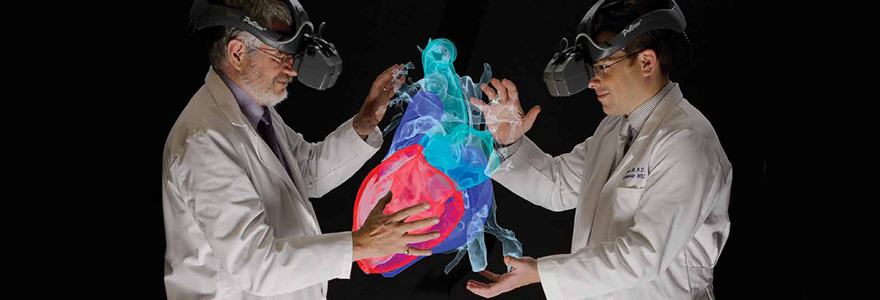
The Virtual Augmentation and Simulation for Surgery and Therapy (VASST) laboratory is concerned with the development and validation of tools that allow surgeons to make efficient use of images, produced by sophisticated 3-D imaging systems, during surgical procedures. The exciting area of research has attracted a multidisciplinary research team with specialized knowledge in fields such as medical imaging, digital image processing, 3D visualization and computer-human interaction.
The objective of minimally-invasive surgery is to improve health or alter the course of
Our lab is focused on minimally invasive procedures as they are applied to:
- The brain
- The beating heart
- The liver, kidney, and prostate
Research Objective
The goal of any ideal image-guided surgery system is to report the position of an intra-operative tool within the brain, heart or
Geometrical inaccuracy of images- Organ and tissue shift between imaging and surgery
- The inability to visualize all of the required information in a single image
- Tracking of instruments with respect to human organs
- The surgeons’ interpretation of the information displayed
We are addressing these problems through research aimed at integrating intra-operative 3-D ultrasound with MRI during surgical guidance, the development of electrophysiological atlases to guide the surgeon during deep brain surgery, the use of computer simulations to guide minimally invasive cardiac and abdominal surgery; the integration of endoscopic images with the previously acquired 3-D volumes; and the development of virtual-reality visualization systems that can present these composite images to the surgeon in the operating room in a simple and intuitive fashion.
Key Questions
- Can integration of pre-operative
aquired - To what extent can a computer simulation of a surgical procedure help the surgeon optimize the operation?
- Can the integration of real-time intra-operative image acquisition effectively complement the use of pre-operative imaging to compensate for tissue shift during surgery?